The technology, developed at the University of Bath, has potential to detect infection earlier, allowing improved treatment for burns patients as well as reducing the use of antibiotics, helping combat the threat of drug-resistant bacteria.
The trial, at Southmead Hospital Bristol, Bristol Royal Hospital for Children, Chelsea and Westminster Hospital and Queen Victoria Hospital East Grinstead will see swabs and used dressings taken from hundreds of patients to be used in laboratory tests at the University of Bath.
These double-blind tests will establish statistically how sensitive the bandages are to infections, and how specifically they react to infections they are designed to detect. The samples will also undergo tests by scientists at the University of Brighton seeking genomic data from infection-causing bacteria which will help improve the bandages’ performance further.
The nature of burns wounds unfortunately means signs and symptoms of infections are common but true infection is rare. A colour-changing bandage will provide an early-warning that infection is developing, allowing better and timelier treatment for patients. It will also prevent unnecessary tests in patients who do not have infection. Existing diagnosis methods take up to 48 hours and require removing wound dressings, a painful and distressing process for the patient which can slow healing and cause scarring.
Currently in cases of suspected infection precautionary courses of antibiotics are often prescribed. The colour-changing bandage would reduce this need, helping tackle the global problem of bacteria developing antibiotic resistance and saving the NHS money on drugs.
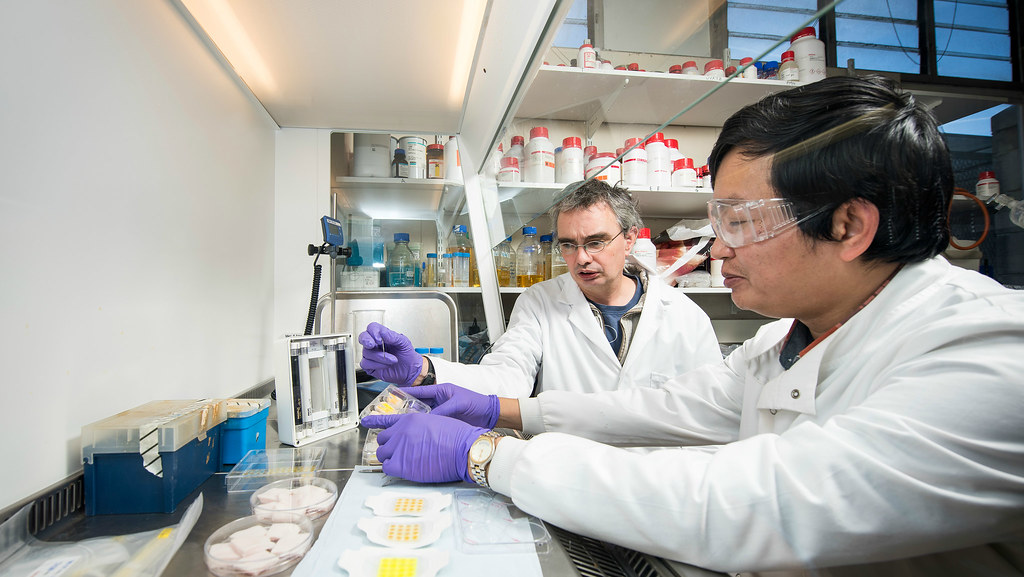
Professor Toby Jenkins, who is leading the study, said: “We believe our bandages have great potential to improve outcomes for patients, reduce unnecessary use of antibiotics and save the NHS money.
“These trials are an exciting and essential step towards getting the bandages into hospitals to help treat people, allowing us to find out exactly how well they work using real samples from patients. We hope as many people as possible agree to take part in the trial, which is completely non-invasive.”
Dr Amber Young, consultant paediatric anaesthetist at Bristol Royal Hospital for Children’s hospital and the lead clinician on the trial, said: “Using patients’ samples to test the dressing's ability to detect infection will take us closer to the use of the dressing in patients.
“Diagnosing wound infection at the bedside in patients with burns will allow targeted treatment of those with true infection; allowing earlier healing and reduced scarring as well as preventing overuse of antibiotics and unnecessary dressing removal in those patients with no infection. This will benefit both patients and the NHS.”
If the trials demonstrate that the bandages are effective then manufacturing could begin as early as next year.
The trial has been funded by the Medical Research Council (MRC).