The MRSA superbug is notorious for going undetected by the body’s immune system, but the mechanisms behind this evasion are poorly understood. Now biologists at the University of Bath have developed a tool that promises to throw light on the pathogen’s tactics by tracking a protein produced by the host’s body after the protein sticks to the microbe.
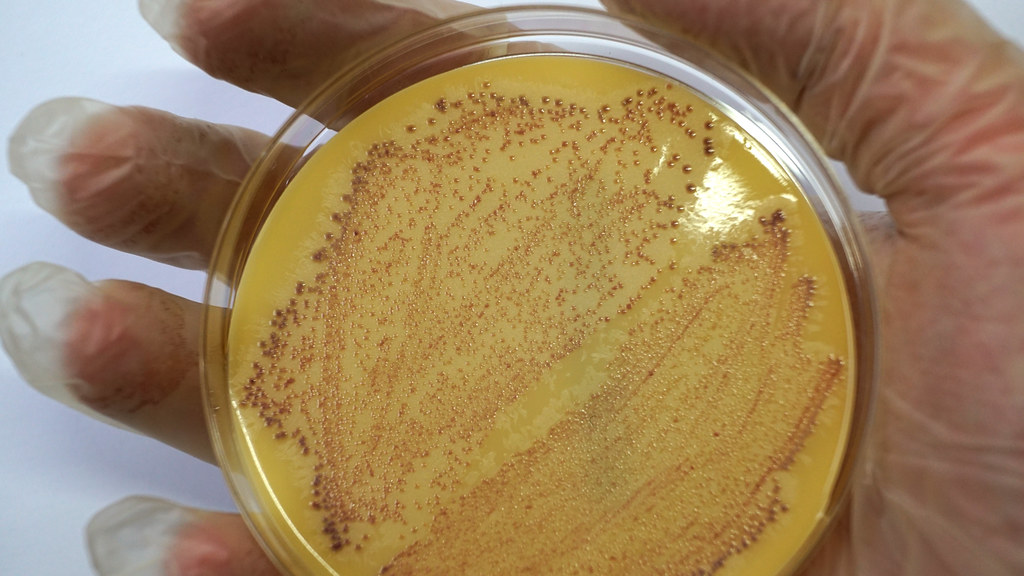
By measuring the levels of this protein on the microbe’s surface, the tool – developed by Dr Maisem Laabei and Professor Jean van den Elsen – promises to help researchers understand how the bacterium Staphylococcus aureus causes disease in humans. In time, it may also help them find new ways to boost a person’s immune system against deadly Methicillin-resistant Staphylococcus aureus (MRSA) and other ‘staph’ infections.
“Understanding how staph interferes with this protein, along with the immune system’s ability to eliminate it from the body, may provide future targets for medical intervention,” said Dr Laabei.
The system that complements the activity of antibodies
The new tool, described in the journal Scientific Reports, measures C3 – a protein belonging to a part of the immune system known as complement. Complement plays a central role in the body’s defence against infection.
When all runs smoothly, the complement system (which includes a group of 50 proteins and protein fragments) springs into action when an invading microbe is first detected. The system enhances (or ‘complements’) the rest of the immune system, surveying the body for intruders, rupturing the cell walls of bacteria and flagging microbes to immune cells, which then go on to eliminate the threat.
All successful pathogens have evolved mechanisms to resist complement, and the more skilful the pathogen is at evading this system, the more potential it has to cause harm to health. S. aureus owns a particularly extensive anti-complement arsenal. As a result, when actors from the complement system land on S. aureus, the cascade of disease-fighting reactions that is supposed to occur on the surface of the pathogen fails to be triggered.
Until now, unpacking the precise sequence of pathogen-led events that blocks complement has been hindered by a lack of tools to accurately measure C3. The detection method developed in Bath is thought to be the first to give a reliably accurate measurement.
“C3 is essential for a successful immune response, so measuring how much is found on the surface of the microbe provides an important insight into the strategies used by the microbe to prevent complement activation,” said Toska Wonfor, the PhD student working on the project.
Damaged organs
A second potential application of the researchers’ new tool involves detecting complement activation in people who have experienced organ damage. Complement is mobilised after the body has suffered an interruption of blood flow to an essential organ – say, as a result of an autoimmune disease (e.g. affecting the kidneys), a stroke or a heart attack.
Professor Van den Elsen said: “When the blood starts to flow again, complement is activated, and the damage to an organ can be understood by measuring the deposition of C3 to the tissue.
“As things stand today, you can only get a good indication of the status of a disease by taking an organ biopsy. We hope our tool will give experts a far less invasive way of exploring what has happened in the body.”
He added: “We’re very excited to see how we can use this tool as an application in the clinic for studying inflammation and autoimmune diseases.”
This project was funded by the Academy of Medical Sciences Springboard Award (SBF006\1023). Ms Wonfor was supported by a University Research Studentship Award from the University of Bath.